Our Approach to Codeveloping an Educational Resource for the LGBTQ+ Community
When creating a brochure for diverse populations of people it’s important to consider an expansive definition of diversity that includes, but is not limited to, ethnic and racial identity. In this case, our intended audience included Lesbian, Gay, Bisexual, Transgender, Queer, Intersex, and Asexual people (LGBTQ+), in addition to all other sexual orientations, gender identities, and gender expressions. Given that sexual identity intersects with every other form of identity, we had to take particular care to ensure that the diverse perspectives of this community were represented in the brochure. In practice, that meant acknowledging and giving space for people to speak about the many identities they inhabit and how those other identities inform their LGBTQ+ experiences.
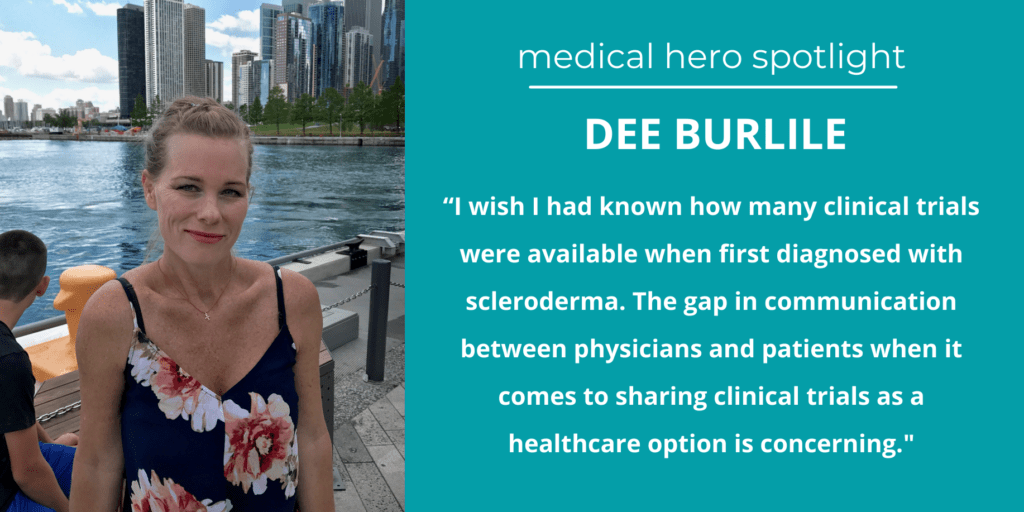
Our discussions with subject matter experts and members of the public from the LGBTQ+ community also showed us that it was most important to give members of this community the tools they needed to navigate clinical trials in a such way that gave them agency and outlined the initial steps for making change by participating in advocacy groups and as members of the public on ethics committees.
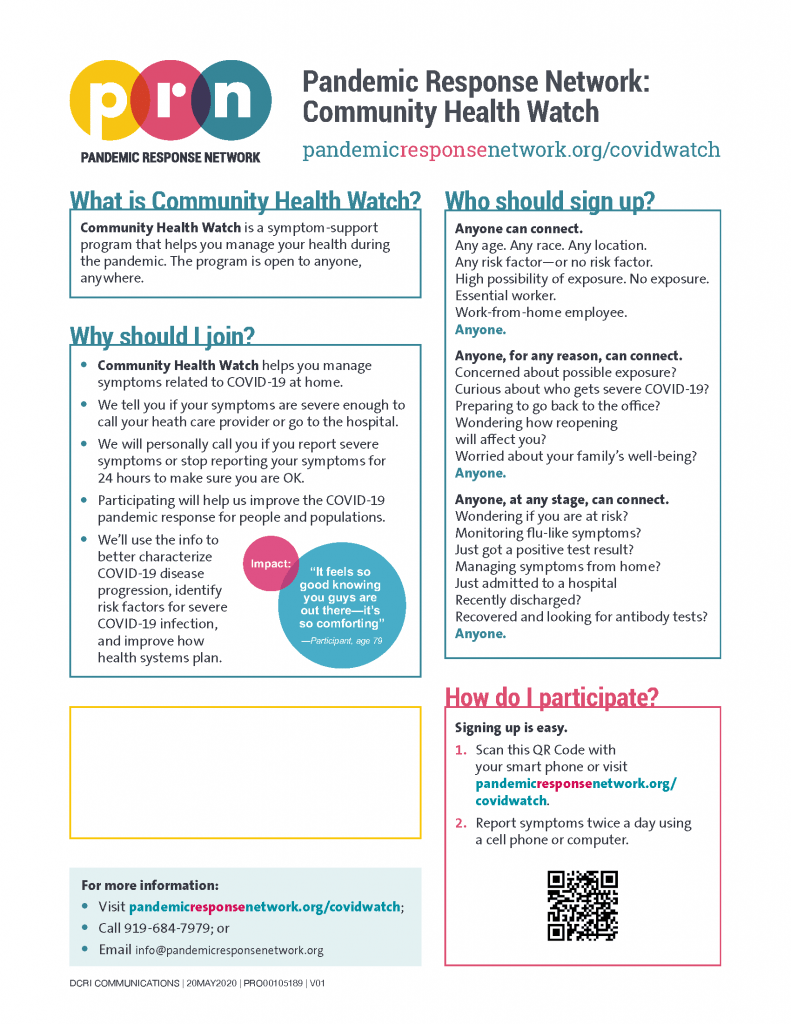
Once we incorporated feedback from the aforementioned SMEs and community members, we tested the brochure with a survey sent to 500 members of the LGBTQ+ community to ensure that the brochure was culturally competent, neutral, and informative. This process helped make sure the topics, language, images, and design are appropriate and engaging. We also received feedback on how effective our brochure was for raising awareness about the importance of LGBTQ+ participation in clinical research.
Key Insights We Learned About Including LGBTQ+ People in Clinical Research
Respondents emphasized that the onus for navigating clinical trials as a member of the LGBTQ+ should be shared: researchers must acknowledge that the determinants of health and the ability to participate in clinical research are multidimensional. For example, one’s lived experience, geographic location, ability to access health services and procedures are also important variables when considering how to make treatments safe and effective for everyone.
To that end, this brochure was created to raise awareness about clinical trials and to identify the barriers to inclusion, and the potential concerns members of the LGBTQ+ community may have with participation in clinical trials. To do this well, we had to consider how history, culture, and even current events may structure a group’s perception of clinical trials. Our initial research with SMEs and community advocates brought up historical wrongs, such as the US federal government’s hostility towards HIV/AIDS research, that have left enduring legacies of mistrust and suspicion towards clinical trials. However, the source of this mistrust isn’t confined to the past: many of our conversations with SMEs centered on current legislation at the state level that targets trans and non-binary people by denying them necessary medical care has likely had a chilling effect on their seeking medical care or clinical trials.
When we spoke about these issues to members of the LGBTQ+ community we received critical feedback that raising awareness was important but insufficient. In order to develop the most helpful version of this brochure, we were asked to highlight the ways in which the lack of action from researchers to be more inclusive negatively impacted access to care, willingness to participate, and the overall experience of participation for those who did partake. They advocated for switching the narrative from one that asked LGBTQ+ people to navigate the pitfalls of clinical trials, to one that also put the onus on researchers to accommodate their needs. Reviewers emphasized that this approach moved the onus of accommodation from participants to researchers.
Next Steps Towards LGBTQ+ Inclusion in Clinical Research
However, there is so much more work to be done. Collaborating with LGBTQ+ communities to raise awareness about representation and inclusion of LGBTQ+ people in clinical research must be an ongoing efforts in all spheres of the clinical research industry, as conditions are continuously changing. In practice, these efforts would include outreach, awareness, and empowerment of the communities with education and resources to help them participate in their own advocacy. In addition to empowering participants, researchers must initiate their own educations to ensure they are adopting more inclusive practices.
Testimonial
It gives me great pleasure to share my testimony on working with the Center for Information & Study on Clinical Research Participation (CISCRP) for a number of years; most recently on their LGBTQ+ brochure project, the development of which I had the incredible privilege of being a small part of. From its very inception, it was clear that this was not just ‘another brochure,’ but a meaningful step towards addressing the long-standing gaps in clinical trial participation and research among the LGBTQ+ community. The journey towards crafting CISCRP’s comprehensive and inclusive resource once again demonstrates not only their ongoing, deep commitment to highlighting the urgent need for further work to ensure genuine inclusion but also to further explore the unique challenges faced by some of the most under-resourced populations in the realm of clinical trials.
The development process, as is always the hallmark of the CISCRP team, was again marked by unwavering dedication, collaborative effort, and an unyielding commitment to authenticity. We had the pleasure and privilege of engaging with community members, medical professionals, and LGBTQ+ advocacy organizations to ensure that every aspect of the brochure resonated with the lived experiences of those for whom it was designed to serve.
This brochure is a tool – a catalyst for change – that has the potential to spark meaningful conversations, challenge preconceptions, and drive research policy reforms. I heartily commend the CISCRP team for recognizing the importance of inclusivity and continuing their critical work to dismantle stigmas, advocate for change, and ensure representation among all individuals at the table – and to empower communities to actively shape the future of clinical research. My journey in helping to develop the LGBTQ+ brochure for CISCRP has been an experience of profound learning, empathy, and hope, and one that reinforces the fact that progress is made through collaboration, compassion, and a relentless pursuit of equality.
This is an endeavor to celebrate, though we must remember that the path ahead is still quite long. I have every confidence that the CISCRP team’s dedication in ensuring every voice is heard, every story is valued, and every individual is embraced within the scientific arena will be resolute. I commend them on, and deeply appreciate, their quest for engaged representation and inclusivity in clinical trials for all. It is a true honor to work with this team and contribute to their meaningful efforts as THE leader in patient engagement, clinical research education, and clinical trial research and participation.
Heather C. Guidone, BCPA, Surgical Program Director
The Center for Endometriosis Care